Competence is an ability with a theoretical basis that can be practically assessed. An individual who achieves competence must have a defined level of theoretical knowledge and the ability to demonstrate a practical application of those skills in a wide range of clinical scenarios.
Emergency Department Nurse Competencies
- Clinical skills
- Communication skills
- Teamwork/collaboration
- Knowledge and scope of practice
- Professional development
- Organisational awareness
- Research
- Quality improvement
- Clinical skills
- Early detection of critical presenting symptoms.
- Assessment of patients based on the Airway, Breathing, Circulation, Disability and Exposure (ABCDE) methodology.
- Initiation of timely nursing interventions in accordance with evidence based clinical pathways and guidelines.
- Continuous assessment and early escalation of care based on clinical knowledge to minimise the risk of deterioration.
- Application of critical thinking skills to recognise and actively participate in the treatment of a wide range of clinical presentations.
- Utilisation of Triage as a dynamic process to ensure continuous prioritisation of patients based on clinical needs.
- Application of the triage process to ensure that the patient is seen within the right time, in the right place by the right caregiver for the right reason.
- Communication
- Communicates effectively and professionally with patients, relatives and the multi-disciplinary clinical team
- Utilisation of available technologies to maximise communication and support patients’ independence and autonomy.
- Communicates with all members of the multi-disciplinary team prioritising a patient centred approach.
- Communicates in a professional manner.
- Delivers clear, concise, accurate and timely communication.
- Teamwork/collaboration
- Co-ordination and participation within the multi-disciplinary team to respond to the patients’ needs based on clinical urgency.
- Recognition and response to all emergency and disaster situations.
- Appropriate initiation of referrals to multi-disciplinary team members or service providers outside the Emergency Department to support individualised patient care.
- Knowledge and scope of practice
- Application of emergency nursing care within individual professional scope of practice and seeks support or guidance as appropriate.
- Actively seeks feedback from colleagues whilst critically reflecting on personal professional nursing practice.
- Professional development
- Has achieved or is working towards a postgraduate qualification in Emergency Nursing.
- Maintains a professional portfolio that includes documented learning and performance goals.
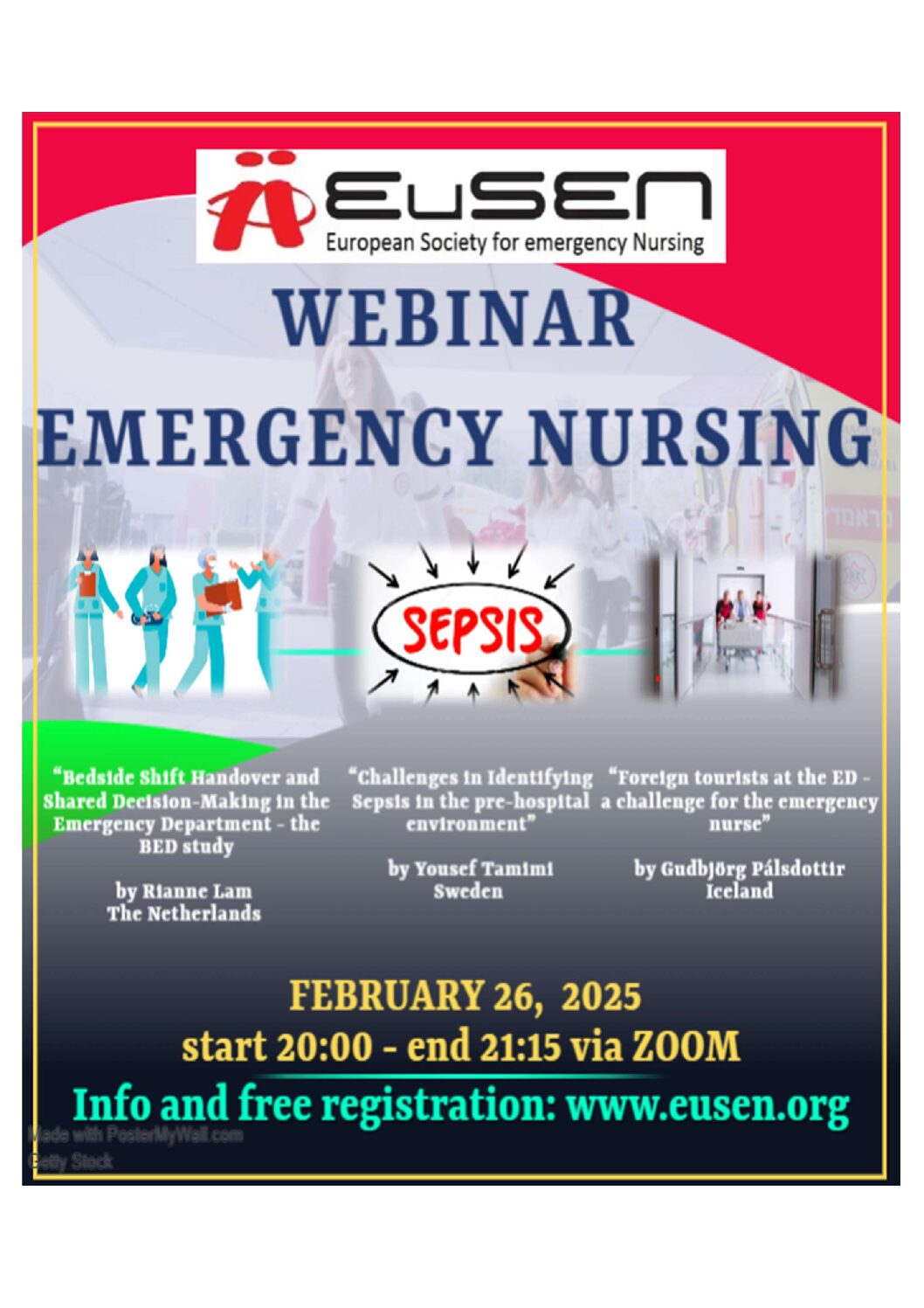
- Participates and contributes to activities or events that enhance the profile of emergency nursing.
- Organisational awareness
- Functions as a professional representative of the Emergency Department.
- Manages space within the Emergency Department to achieve maximum efficiency and optimise patient flow.
- Proactively manages patient flow to minimise the impact of access block and to optimise patient safety.
- Actively maintains and supports professional networks both inside and outside their healthcare organisation.
- Demonstrates a thorough working knowledge of departmental and organisational policies and procedures.
- Research
- Participates in and supports research that promotes emergency nursing.
- Promotes a culture of research and evidence based practice within the emergency nursing care profession.
- Quality improvement
- Takes personal responsibility for professional development.
- Actively contributes to the development of professional standards in Emergency Nursing.
- Promotes and participates in a culture of continuous quality improvement within the emergency nursing profession.
*Nursing interventions
A/B: Assessment of airways and breathing. Administration of oxygen, nasal, oral or inhalational medications (nursing standing orders).
C: Assessment of circulation, intravenous (IV) cannula insertion, administration of IV medications and completion of an Electrocardiograph (ECG).
D: Collection of the patient’s vital signs, blood sugar level (BSL) and Glasgow Coma Scale (GCS).
E: Completion of a full body check (head to toe), clinical assessment and application of casts or wound dressings.
Others:
Collection of blood or urine samples, insertion of urinary catheter, ordering of limb X-rays as appropriate.
References:
Learning outcomes for a bachelor in Emergency care; presentation Maria Deneire 2014 (Belgium)
NENA standards and practice Emergency core competencies 2014 (Canada)
CENA practice standards for the Emergency Nursing Specialist 2013 (Australia)
Areas of expertise and attainment targets for Emergency nursing care (The Netherlands)
ICN Nursing care continuum framework and competencies